The Connection Between the Gut and Mental Health
Your Gut and Mental Health
Your gut houses trillions of bacterial cells of about 500 to 1,000 different species. Believe it or not, this bacteria can actually help with symptoms of stress, anxiety, and depression or make it worse. So, let's take a look at how this works.
Have you ever had a gut feeling or butterflies flurrying in your tummy?
Well, these sensations you feel in your belly actually suggest that your gut and brain are connected.
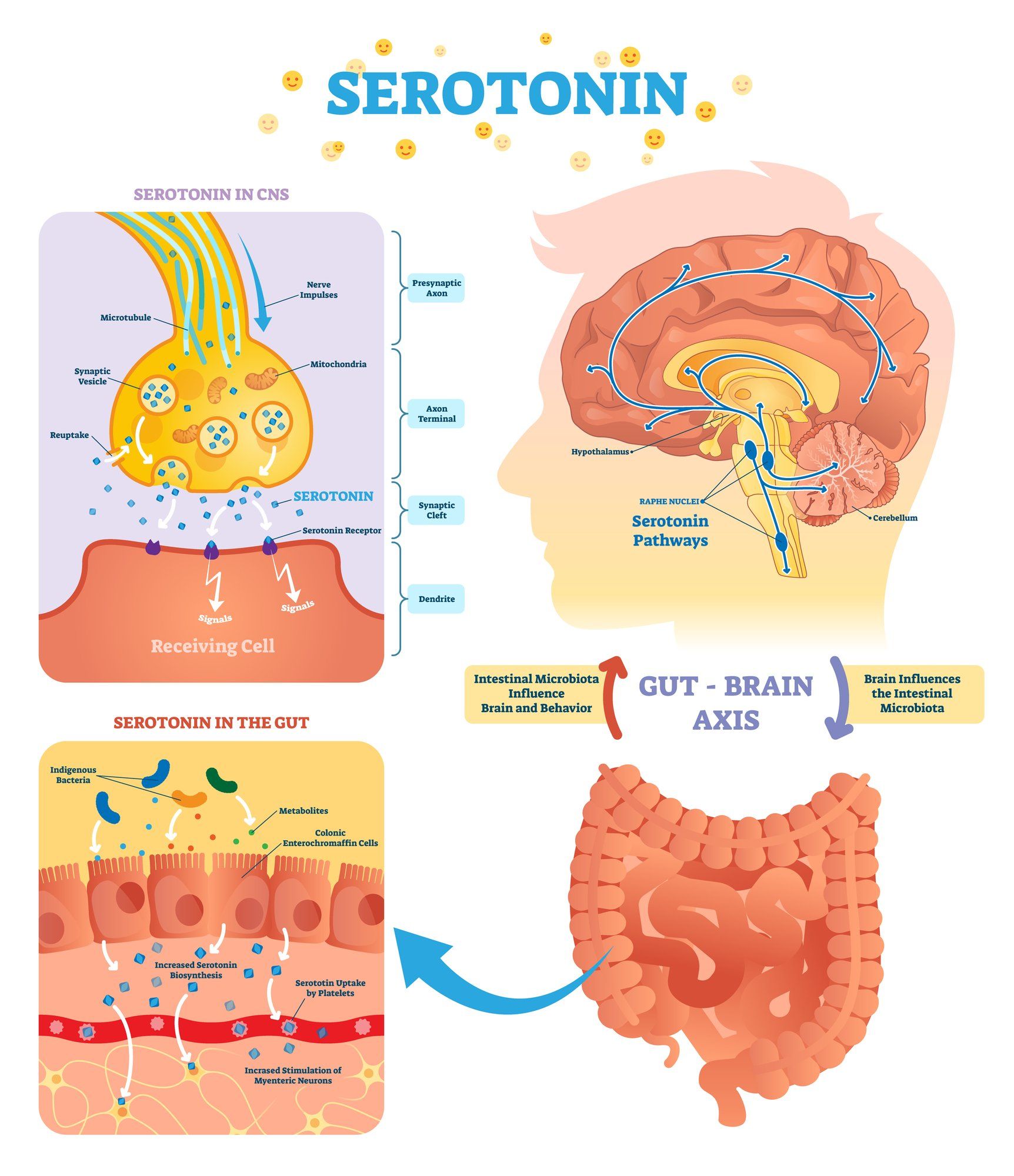
To confirm, many studies show that your brain does affect your gut health and vice versa. This is referred to as your gut-brain axis, which is the communication network that connects your gut to your brain.
Your Nervous System
Neurons are fundamental units of the brain and central nervous system. Their role is to tell our body how to behave. Neurons are essentially responsible for receiving information from the world around you, sending commands to your muscles, and transforming and relaying electrical signals.
Do you know which nerve is the largest one in your body. That's right, the vagus nerve.
Interestingly enough, it connects the gut to the brain and sends signals in both directions. The vagus nerve has a lot of responsibility, including the regulation of bodily organs. In fact, by stimulating the vagus nerve, you can send a message to your body to relax, calm yourself, and de-stress your mind and body. Poor mental health, such as stress, depression, and anxiety are symptoms of a poorly regulated nervous system. This occurs as our response to environmental stressors (i.e., trauma, etc.) either becomes excessive (causing fear, anxiety, nervousness, or panic attacks) or down-regulated (causing depression, sadness, apathy, etc.). This equates to poor vagus nerve function. So, it makes sense, that by increasing your vagal tone, it provides an opportunity to assist you with overcoming stress, anxiety, and a depressed mood.
Neurotransmitters
Neurotransmitters also connect the gut to the brain. Neurotransmitters are technically chemical substances that are produced specifically to transmit messages between neurons (i.e. chemical messengers). For example, some of the major neurotransmitters include, acetylcholine, dopamine, gamma-aminobutyric acid (GABA), glutamate, histamine, norepinephrine, and serotonin.
Norepinephrine is a stress hormone released into the blood that functions as a neurotransmitter in the central nervous system. Reduced neurotransmission of norepinephrine can result in low energy levels, difficulties with attention and concentration, lessened alertness, and a decreased cognitive ability.
While serotonin is produced in the brain where it performs its primary function, nearly 90% of it is found in the gut (digestive tract) and in blood platelets. From the near 40 million brain cells, most of them are influenced in either directly or indirectly from serotonin. These include brain cells that are related to mood, appetite, sleep, sexual function, memory and learning, and social behavior. This explains why research indicates that low levels of serotonin are attributed to many of the symptoms of depression and anxiety, and even obsessive compulsive disorder (OCD).
The Connection between the Gut and Mental Health
When we consider what we've learned about the connection between the brain and the gut, we can understand how serotonin and digestion work hand in hand. Our entire well-being is centered around the gut! When the levels of serotonin are insufficient in the gut, you will likely experience both physical and mental symptoms. Physically, you may have diarrhea or constipation, bloating, or cramping. Mentally, you may experience sleeping problems and symptoms associated with depression and anxiety.
Eating a healthy, well-balanced diet, rich in veggies and fiber can help maintain sufficient serotonin levels. So stock up on a variety of vegetable, fruits, fish, lean meats, whole grains, and complex carbohydrates. And, be sure to cut way back on processed foods, fast food, refined sugars and carbohydrates, and minimize your caffeine and alcohol intake.